Typical Treatment
– Azoospermia
Obstructive Azoospermia
Azoomspermia is a disorder in which there is a complete absence of sperm in the semen. There are two types of Azoospermia: Obstructive and Non-obstructive.
A clear example of “intentional” Obstructed Azoospermia is a vasectomy. A vasectomy is a procedure in which the tube that carries the sperm from the testis to the penis (vas deferens) is surgically cut as an intended form of birth control. In this example the path of the sperm out of the body is prevented and therefore obstructed. Other than in this case, Obstructive Azoospermia is usually not desired yet the infertility mechanism is very similar to a vasectomy. Obstructed Azoospermic men usually have the ability to produce healthy and active sperm but an obstruction prevents it from traveling out of the body. The positive aspect of this is that healthy sperm are produced and can easily be removed from the epididymis (the small oblong body which is attached to the back of each testis) for use through Epi didymal Sperm Aspiration.
Treatmet using Epididymal Sperm
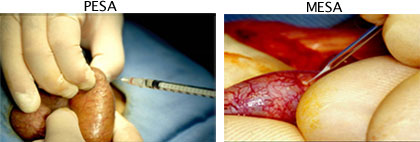
 There are two different methods of Epididymal Sperm Aspiration. One method is done by withdrawing the sperm directly out of the epididymis by needle aspiration through the skin of the scrotum (see the image on the left- Percutaneous Epididymal Sperm Aspiration (PESA)). The second method is to make an incision through the scrotum, expose the epididymis so it can be clearly seen, and then collect the sperm (see the image on the right – Microsurgical Epididymal Sperm Aspiration (MESA)). A one-day stay at our hospital is required for this procedure. Although the percutaneous method (PESA) (through the skin) does not require surgery we recommend the second method (MESA) since it is more effective for collecting larger amounts of healthy sperm.
There are two different methods of Epididymal Sperm Aspiration. One method is done by withdrawing the sperm directly out of the epididymis by needle aspiration through the skin of the scrotum (see the image on the left- Percutaneous Epididymal Sperm Aspiration (PESA)). The second method is to make an incision through the scrotum, expose the epididymis so it can be clearly seen, and then collect the sperm (see the image on the right – Microsurgical Epididymal Sperm Aspiration (MESA)). A one-day stay at our hospital is required for this procedure. Although the percutaneous method (PESA) (through the skin) does not require surgery we recommend the second method (MESA) since it is more effective for collecting larger amounts of healthy sperm.
When sperm is not found in the epididiymis
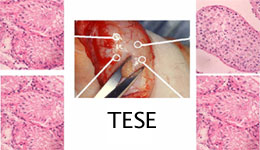
In some cases some azoospermic men do not have any sperm at all in their epididymis. In this case, a small amount of testicular tissue is biopsied. This tissue is then manipulated to disentangle the seminiferous tubule. These seminiferous tubules are then examined with a microscope to find any sperm that are moving within. Intra cytoplasmic sperm injection (ICSI) can then be performed with these sperm to induce pregnancy. Even in cases of where Epididymal Sperm Aspiration is not possible, or when there is no sperm in the testis, all hope is not lost since there is still the possibility of pregnancy.

Non-obstructive Azoospermia:
Non-obstructive Azoospermia is the condition where the testis itself has a production ability disorder and therefore is unable to produce mature sperm. Even in this case pregnancy may still be possible. To accomplish this a small amount of tissue needs to be removed from the testis, which is then analyzed under a microscope to see if there are any testicular sperm contained within it. If found, these sperm are retrieved for Intra Cytoplasmic Sperm Injection (ICSI).
Spermatids:
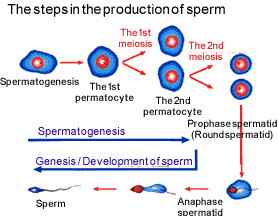 Even in cases where no mature sperm can be found in the testis of azoospermic men, about 30% of these men still have produced late-staged spermatids that are contained in their testis. A late-staged spermatid is an undeveloped sperm that is one stage prior to becoming a fully developed sperm. For these cases, it may be possible to conceive using these late-staged spermatids through ICSI (Intra cytoplasmic sperm injection). There are 2 basic spermatid types, round spermatids and late-stage spermatids. An early stage spermatid that has a round nucleus (center) is called a round spermatid, and when a spermatid starts to become elongated it is then called a late-stage spermatid. Although the rate of successful pregnancies when using late-stage spermatids is comparable to that of mature sperm there may be risks when using these immature cells and safety cannot be guaranteed 100% of the time. The first successful treatment of infertility using late-stage spermatids at our hospital was over 7 years ago. This is a relatively short period of time so that it is yet unknown if there are any delayed side effects from this treatment. Until now we have not seen any reports of child onset problems associated with this treatment, although there does appear to be risk that a male child may also become azoospermic. Reports have suggested that azoospermia may not only be a chromosomal problem but may be a genetic problem. We recommend that those who are concerned have a chromosomal analysis and genetic exam done. For patients who desire this treatiment option, we will explain the risks and benefits involved with treatment using immature spermatids.
Even in cases where no mature sperm can be found in the testis of azoospermic men, about 30% of these men still have produced late-staged spermatids that are contained in their testis. A late-staged spermatid is an undeveloped sperm that is one stage prior to becoming a fully developed sperm. For these cases, it may be possible to conceive using these late-staged spermatids through ICSI (Intra cytoplasmic sperm injection). There are 2 basic spermatid types, round spermatids and late-stage spermatids. An early stage spermatid that has a round nucleus (center) is called a round spermatid, and when a spermatid starts to become elongated it is then called a late-stage spermatid. Although the rate of successful pregnancies when using late-stage spermatids is comparable to that of mature sperm there may be risks when using these immature cells and safety cannot be guaranteed 100% of the time. The first successful treatment of infertility using late-stage spermatids at our hospital was over 7 years ago. This is a relatively short period of time so that it is yet unknown if there are any delayed side effects from this treatment. Until now we have not seen any reports of child onset problems associated with this treatment, although there does appear to be risk that a male child may also become azoospermic. Reports have suggested that azoospermia may not only be a chromosomal problem but may be a genetic problem. We recommend that those who are concerned have a chromosomal analysis and genetic exam done. For patients who desire this treatiment option, we will explain the risks and benefits involved with treatment using immature spermatids.