PGD / PGS
Preimplantation Genetic Diagnosis (PGD)
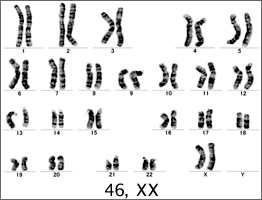
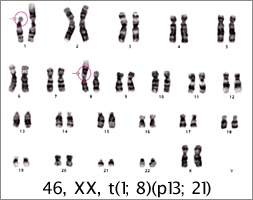
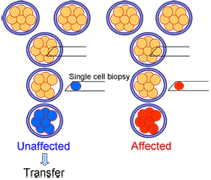 Preimplantation genetic diagnosis (PGD) is an early alternative to prenatal diagnosis and is suitable for patients who are at substantial risk of conceiving a pregnancy affected by a known genetic defect. The technique has been applied to the analysis of numerical and structural chromosomal abnormalities that can result in handicap or recurrent pregnancy loss, the identification of sex to prevent transmission of X linked disease, and for the detection of specific serious monogenic disorders.A single blastomere is removed from each 8-cell human embryo for the purposes of preimplantation genetic diagnosis. Up to two embryos found to be unaffected by the genetic disorder are transferred to the uterus.
Preimplantation genetic diagnosis (PGD) is an early alternative to prenatal diagnosis and is suitable for patients who are at substantial risk of conceiving a pregnancy affected by a known genetic defect. The technique has been applied to the analysis of numerical and structural chromosomal abnormalities that can result in handicap or recurrent pregnancy loss, the identification of sex to prevent transmission of X linked disease, and for the detection of specific serious monogenic disorders.A single blastomere is removed from each 8-cell human embryo for the purposes of preimplantation genetic diagnosis. Up to two embryos found to be unaffected by the genetic disorder are transferred to the uterus.
PGD for nomogenic diseases:
| Autonomal recessive (No of referrals) |
Autosomal dominant (No of referrals) |
X-linked (No of referrals) |
| CF (109) | Myotonic dystrophy (88) | Fragile X (75) |
| Thalassemia (53) | Huntington’s disease (73) | DMB / BMD (69) |
| SMA (50) | CMT (20) | Hemophilia (26) |
| Other (78) | Other (73) | Other (73) |
| Total (290) | Total (254) | Total (294) |
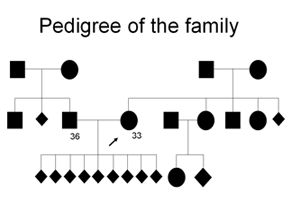
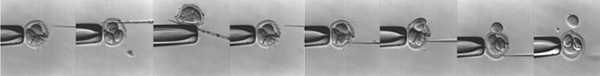
Procedure of embryo extrusion:
Preimplantation Genetic Screening (PGS)
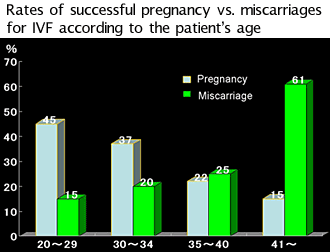
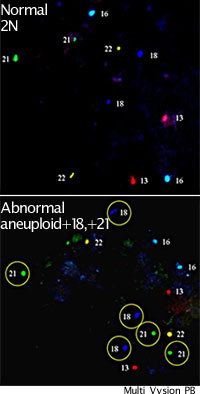 Some women, including those in older age groups (>38 years) and those who have had repeated failure of in vitro fertilisation, are more likely to produce cytogenetically abnormal embryos, which are not capable of normal development. For these patients, preimplantation genetic screening or aneuploidy screening has been advocated.
Some women, including those in older age groups (>38 years) and those who have had repeated failure of in vitro fertilisation, are more likely to produce cytogenetically abnormal embryos, which are not capable of normal development. For these patients, preimplantation genetic screening or aneuploidy screening has been advocated.
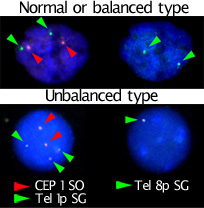
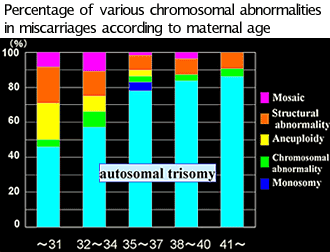
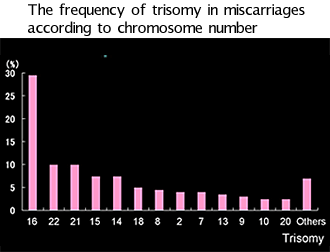
By using techniques developed for PGD to select normal embryos, the chromosomes that are responsible for the major survivable aneuploidies (for example, 21, 22, 18, 13, X, and Y) can be examined from an embryo biopsy using fluorescence in situ hybridization.
As over half of all embryos can be cytogenetically abnormal, excluding these embryos from selection has improved ongoing implantation rates in some studies. However, the restriction to the common aneuploidies still allows those embryos that may have other chromosomal rearrangements to remain undetected. This limits the usefulness of the screening.
References:
Rate of embryos in category
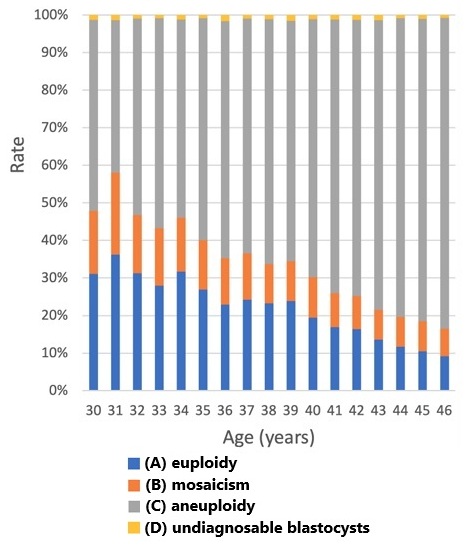
Numbers and rates of euploidy (A), mosaicism (B), aneuploidy (C), and undiagnosable blastocysts (D), stratified by maternal age.
Data of embryos in all categories (RIF, RPL, and CR) are included. CR, chromosomal structural rearrangement; RIF, recurrent implantation
failure; RPL, recurrent pregnancy loss.
Reference:
Iwasa T et al. Preimplantation genetic testing for aneuploidy and chromosomal structural rearrangement: A summary of a nationwide study by the Japan Society of Obstetrics and Gynecology. Reprod Med Biol. 2023 May 31;22(1):e12518.
The number of eggs stored required to obtain a normal embryo for a given age. category
| age | 38 | 39 | 40 | 41 | 42 | 43 | 44 | 45 |
| 4~5 | 5~6 | 5~6 | 6~7 | 6~7 | 7~8 | 8~10 | 10 | |
| Probability of finding a normal embryo (A). | 23% | 24% | 19% | 17% | 17% | 14% | 12% | 10% |
*Precautions.
The pregnancy rate for each normal (A) embryo is approximately 50%.
Transferring a normal embryo does not guarantee 100% pregnancy and delivery.